In the ever-evolving field of medical science, stents have emerged as a groundbreaking solution for treating various health conditions. These small, flexible mesh-like tubes have revolutionized the way we manage and address cardiovascular, vascular, and other related ailments. Through step-by-step guides, we will provide valuable insights into the stent placement, removal, and insertion procedures, ensuring a better understanding for patients and caregivers alike. Additionally, we will explore the management of stent complications, address issues like stent migration and thrombosis, and delve into the latest innovations and advancements in stent technology.
Join us on this captivating journey as we unlock the potential of stents and their transformative role in modern medicine. In partnership with Medzell, a futuristic B2B platform promoting Indian medical devices in emerging markets, we strive to provide you with the most up-to-date information and empower you with knowledge that can positively impact patient care.
Understanding Stents
Stents are small, tube-like devices commonly used in medical procedures to treat and manage various conditions in the body’s blood vessels and organs. They are also utilized in peripheral vascular interventions to treat arterial diseases affecting the blood vessels outside of the heart, such as the legs, arms, or kidneys. They help alleviate symptoms, restore blood flow, and prevent further complications in patients with conditions like peripheral artery disease. Also, stents are used in the biliary and urinary systems to address obstructions or strictures in the bile ducts and ureters, respectively. By placing stents in these areas, normal flow is restored, providing relief to patients and preventing complications. Esophageal stents are employed in the management of esophageal conditions, such as strictures or tumors, to improve swallowing and alleviate symptoms. They have revolutionized medical interventions by offering minimally invasive solutions that can often replace the need for more invasive surgeries. They have significantly improved patient outcomes and quality of life by providing effective treatment options with shorter recovery times.
Exploring Different Types of Stents
Stents play a vital role in the medical field, offering a minimally invasive solution for treating various conditions involving blocked or narrowed blood vessels or ducts. Following are the different types of Stents.
- Coronary Stents: These stents come in different types, including bare metal stents (BMS), drug-eluting stents (DES), and bioresorbable stents. BMS provides support to the vessel structure, while DES releases medication to prevent the recurrence of blockages. On the other hand, bioresorbable stents gradually dissolve over time, allowing the artery to heal naturally.
- Peripheral Stents: Peripheral stents are a specialized type of stents used for treating blockages in arteries located outside the heart, including the legs, arms, or neck. They come in two main designs: self-expanding and balloon-expandable. Self-expanding stents are crafted from a remarkable shape-memory alloy called nitinol, enabling them to naturally expand and conform to the vessel walls.
- Biliary Stents: Biliary stents are utilized to treat obstructions in the bile ducts caused by conditions like gallstones, tumors, or strictures. These stents are often made of metal or plastic and help restore the flow of bile from the liver to the small intestine.
- Ureteral Stents: They are frequently used to help manage urinary blockages, such as those caused by kidney stones or narrowings in the ureter. By providing support and improving urine flow, ureteral stents help alleviate symptoms and promote better urinary function.
- Esophageal Stents: These stents are typically designed to expand on their own once in place and are commonly made of either metal or silicone materials. By providing structural support and widening the esophageal passage, these stents assist in restoring normal function and enhancing the overall quality of life for individuals affected by esophageal conditions.
Each type of stent is designed to address specific medical conditions and has its unique characteristics. The selection of the most appropriate stent depends on factors such as the location of the blockage, the patient’s anatomy, and the desired treatment outcomes.
Step-by-Step Guide to Stent Placement Procedure
The stent placement procedure is a minimally invasive intervention performed by healthcare professionals to treat various medical conditions.
- Preparation: At first the patient is prepared by cleansing the insertion site and administering local anesthesia to ensure comfort throughout the process.
- Accessing the Treatment Area: A small incision is made at the insertion site, and a catheter is inserted into the blood vessel or organ where the stent is needed. The catheter is guided to the treatment area using imaging techniques such as X-ray or fluoroscopy.
- Positioning the Stent: Once the catheter reaches the desired location, the stent is carefully advanced through the catheter and positioned at the site of the blockage or narrowing. The stent is designed to expand and conform to the shape of the vessel or organ, providing support and improving blood flow.
- Deployment and Expansion: The stent is deployed by either balloon angioplasty or self-expanding mechanisms. In balloon angioplasty, a balloon at the tip of the catheter is inflated, expanding the stent and pressing it against the vessel walls. In self-expanding stents, the stent expands automatically once released from the catheter.
- Confirmation and Finishing: After the stent is properly positioned and expanded, the healthcare team ensures its correct placement using imaging techniques. The catheter is then removed, and the insertion site is typically closed with sutures or adhesive strips.
- Recovery and Follow-up: Following the procedure, the patient is closely monitored for a period to ensure stability. Pain medications and post-procedure care instructions are provided. Follow-up appointments are scheduled to assess the stent’s effectiveness and monitor the patient’s condition.
It’s important to note that each stent placement procedure may vary depending on the specific medical condition and individual patient factors. The healthcare team will tailor the procedure accordingly to achieve the best possible outcomes.
Step-by-Step Guide to Stent Removal Procedure
Stent removal is a medical procedure performed to safely retrieve a previously implanted stent when it is no longer needed or has served its purpose.
- Preparation: Before the procedure, the patient’s medical history and the reason for stent removal are reviewed. Local anesthesia or sedation may be administered to ensure comfort during the procedure.
- Accessing the Stent: A healthcare professional accesses the stent by locating the insertion site and gently inserting a specialized instrument or catheter into the area where the stent is located. This is typically done under fluoroscopy or imaging guidance to ensure precision.
- Engaging the Stent: The instrument is carefully manipulated to engage the stent. Depending on the type of stent and its location, the healthcare professional may use techniques such as grasping, snaring, or capturing the stent to secure it for removal.
- Retrieval and Removal: Once the stent is securely engaged, it is slowly and gently withdrawn from the body. The process is performed with utmost care to avoid any damage to the surrounding tissues or organs.
- Confirmation and Finishing: After the stent is successfully removed, the insertion site is inspected for any signs of bleeding or complications. The site may be closed with sutures or adhesive strips as necessary. Post-procedure care instructions and pain management techniques are provided.
- Recovery and Follow-up: The patient is monitored closely after the procedure to ensure stability. Follow-up appointments are scheduled to assess healing, address any concerns, and evaluate the patient’s condition.
It’s important to emphasize that stent removal procedures should only be performed by trained healthcare professionals. Proper evaluation and planning are essential to ensure a safe and successful stent removal process.
Managing Stent Complications
While stents are generally safe and effective, complications can sometimes occur. Here are some strategies for managing stent-related complications:
- Early Recognition and Intervention: Promptly identifying stent-related complications is crucial for effective management. Healthcare professionals closely monitor patients after stent placement and assess for signs and symptoms of complications, such as excessive bleeding, infection, or stent blockage.
- Medication Adjustment: Depending on the complications involved necessary adjustments need to be taken. It may involve changes in antiplatelet therapy, anticoagulant therapy, or other medications to reduce the chances of clot formation and infection.
- Endoscopic Interventions: In cases of stent-related complications involving the gastrointestinal tract or biliary system, endoscopic procedures may be employed. These procedures can help address issues such as stent migration, blockage, or tissue in growth.
- Additional Interventions: In more severe cases, additional interventions may be required. This can involve surgical procedures to resolve complications such as stent thrombosis, stent fracture, or vessel perforation.
- Patient Education and Follow-up: Proper patient education plays a vital role in managing stent complications. Patients should be advised about identifying the complications and steps to take when they arise. Regular follow-up appointments allow healthcare professionals to monitor the patient’s condition and address any concerns promptly.
It’s important to note that the management of stent complications requires individualized care and close collaboration between the patient and healthcare professionals. By promptly recognizing and addressing complications, optimal patient outcomes can be achieved.
Addressing Stent Migration
Stent migration occurs when a stent moves from its intended position within the body. Although relatively rare, it can lead to complications. Following are some approaches to addressing stent migration:
- Conservative Management: In cases where the migrated stent is not causing significant symptoms or complications, a conservative approach may be adopted. Close monitoring, regular follow-up visits, and imaging studies are conducted to ensure the stent’s stability and assess its impact on surrounding tissues.
- Endoscopic Retrieval: In situations where the migrated stent poses a risk or causes symptoms, endoscopic procedures may be employed to retrieve or reposition the stent. This involves using specialized instruments, such as graspers or snares, to capture and remove the migrated stent or reposition it to its original location.
- Surgical Intervention: In rare cases where conservative or endoscopic measures are unsuccessful or not feasible, surgical intervention may be necessary. Surgeons can perform procedures to retrieve or reposition the stent while minimizing damage to surrounding structures.
- Preventive Measures: To reduce the risk of stent migration, proper stent selection and sizing are crucial. Healthcare professionals carefully consider factors such as vessel anatomy, stent design, and patient characteristics during stent placement to minimize the likelihood of migration.
Addressing stent migration requires a case-by-case approach based on specific circumstances and patient factors. Early detection, appropriate evaluation, and collaboration between healthcare professionals from different specialties contribute to effective management and positive patient outcomes.
Managing Stent Thrombosis
When blood clots form within a stent, it can impede blood flow and result in complications called stent thrombosis. Let’s see some ways to manage stent thrombosis.
- Dual Antiplatelet Therapy (DAPT): For certain high-risk patients or complex stenting procedures, DAPT combining two antiplatelet medications may be prescribed. The duration of DAPT varies depending on the type of stent and individual patient factors.
- Lifestyle Modifications: Lifestyle changes can play a role in preventing stent thrombosis. Patients are advised to stop smoking and maintain a healthy weight. These modifications contribute to overall cardiovascular health and reduce the risk of clot formation.
- Regular Follow-up and Monitoring: Close monitoring of patients after stent placement is crucial to detect early signs of stent thrombosis. Regular follow-up appointments allow healthcare professionals to assess the patient’s condition, review medication regimens, and evaluate the stent’s patency.
Proactive management of stent thrombosis involves a combination of medication adherence, lifestyle modifications, and close monitoring. Collaboration between patients, healthcare professionals, and specialized cardiac teams is vital for the successful prevention and management of this potentially serious complication.
Exploring Latest Stent Innovations
In the rapidly evolving field of medical devices, stent technology continues to advance, bringing forth innovative designs and materials. These latest stent innovations aim to improve patient outcomes, enhance safety, and provide more effective treatment options. One notable advancement is the development of bioresorbable stents. Unlike traditional stents that remain in the body permanently, bioresorbable stents gradually dissolve over time, allowing the blood vessel to regain its natural function. Another exciting innovation is the introduction of drug-eluting stents. These stents are coated with medications that are slowly released into the surrounding tissue, helping to prevent the recurrence of blockages and reduce the need for repeat procedures. Additionally, there have been advancements in stent imaging technology, enabling better visualization and precise placement during procedures. The ongoing research and development in stent innovations hold great promise for further improving patient care and expanding treatment options for a wide range of medical conditions.
Long-Term Effects of Stent Placement
Long-term stent placement can have implications for patients, both in terms of efficacy and potential complications. Over time, stents can develop a condition called in-stent restenosis, where the treated blood vessel becomes narrowed again. This can lead to recurrent symptoms and may require additional interventions. To mitigate these risks, patients who have received stents are often prescribed antiplatelet medications to prevent blood clot formation. Regular follow-up visits with healthcare professionals are crucial to monitor the stent’s function and address any potential issues promptly.
Comparing Different Stent Types
When it comes to selecting Stents various factors need to be considered. Bare metal stents, for instance, offer structural support but may have a higher risk of in-stent restenosis compared to drug-eluting stents. Drug-eluting stents, on the other hand, are effective at reducing restenosis rates but may require longer-term use of antiplatelet medications. Bioresorbable stents provide a temporary solution, gradually dissolving over time, but their use is limited to specific cases. In terms of peripheral stents, self-expanding stents offer ease of deployment and adaptability to vessel contours, while balloon-expandable stents provide controlled and precise expansion. The choice between these types depends on the specific requirements of the procedure and the patient’s anatomy. Similarly, biliary, ureteral, and esophageal stents have unique features and considerations. The selection of the appropriate stent type should be made in consultation with healthcare professionals, considering the specific medical condition, potential risks, and desired outcomes.
Stents from Leading Indian Manufacturers
JAVASTENT Tracheal/Bronchial Stent
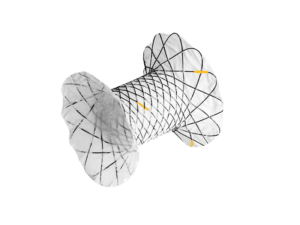
 Introducing the JAVASTENT Tracheal/Bronchial Stent by Medorah Meditek Pvt. Ltd., the leading Indian manufacturer, and global supplier. This advanced stent effectively treats tracheobronchial strictures caused by benign or malignant conditions. Featuring a silicone coating, closed-cell structure, and rounded ends, it prevents tissue ingrowth and minimizes harm. The flared ends ensure stability and prevent migration. With optimal radial force and minimal axial force, the stent adapts to the patient’s lumen. Gradual expansion, facilitated by a hook and cross-construction, ensures a precise fit. Radiopaque platinum markers enable accurate imaging, and repositioning is possible up to 75% deployment. Experience innovation and excellence with the JAVASTENT for improved respiratory function and quality of life.
Introducing the JAVASTENT Tracheal/Bronchial Stent by Medorah Meditek Pvt. Ltd., the leading Indian manufacturer, and global supplier. This advanced stent effectively treats tracheobronchial strictures caused by benign or malignant conditions. Featuring a silicone coating, closed-cell structure, and rounded ends, it prevents tissue ingrowth and minimizes harm. The flared ends ensure stability and prevent migration. With optimal radial force and minimal axial force, the stent adapts to the patient’s lumen. Gradual expansion, facilitated by a hook and cross-construction, ensures a precise fit. Radiopaque platinum markers enable accurate imaging, and repositioning is possible up to 75% deployment. Experience innovation and excellence with the JAVASTENT for improved respiratory function and quality of life.
Stent Pusher
 Experience the precision and reliability of the Stent Pusher by Medinova Endosys, a global leader in endoscopic devices and accessories. Specifically designed for endoscopic biliary stent placement, this individually packed device ensures convenience and hygiene during procedures. With its intuitive color coding system, distinguishing between guider, stent, and pusher becomes effortless, streamlining the workflow and reducing errors. The Stent Pusher is compatible with straight, single-pigtail, and double-pigtail plastic stents, offering versatility for tailored interventions. Medinova Endosys upholds stringent quality standards, accredited by the Indian FDA and ISO 13485:2016 while adhering to guidelines set by the Indian CDSCO. Trust in Medinova’s expertise and certifications to enhance patient outcomes in endoscopic procedures.
Experience the precision and reliability of the Stent Pusher by Medinova Endosys, a global leader in endoscopic devices and accessories. Specifically designed for endoscopic biliary stent placement, this individually packed device ensures convenience and hygiene during procedures. With its intuitive color coding system, distinguishing between guider, stent, and pusher becomes effortless, streamlining the workflow and reducing errors. The Stent Pusher is compatible with straight, single-pigtail, and double-pigtail plastic stents, offering versatility for tailored interventions. Medinova Endosys upholds stringent quality standards, accredited by the Indian FDA and ISO 13485:2016 while adhering to guidelines set by the Indian CDSCO. Trust in Medinova’s expertise and certifications to enhance patient outcomes in endoscopic procedures.
Biliary-Stent
The Biliary-Stent by Aurus MedTech Pvt. Ltd. is a trusted medical device designed to alleviate biliary obstruction by efficiently draining bile from obstructed biliary ducts. With compatibility for guide wires of varying sizes (0.035″, 0.032″, and 0.025″), this versatile stent is available in four different variants, tailored to meet individual patient needs. Crafted from high-quality materials, it ensures durability and long-lasting relief. In certain cases, the Biliary-Stent can serve as an alternative to surgical intervention, offering an effective treatment option. Proper placement and removal procedures are crucial to ensure safety and efficacy, while comprehensive management of complications is essential for optimal results. The lifespan of the stent depends on factors such as the stent type, patient condition, and level of obstruction, with potential replacement needed for obstructions, infections, or changes in the patient’s condition.
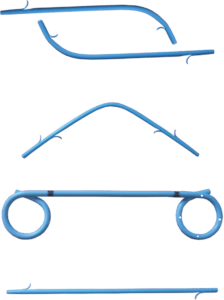
Biliary Stent (Pigtail, Straight, Curved)
MEDITECH DEVICES PVT LTD, a renowned manufacturer and supplier from India, offers the highly efficient Biliary Stent (Pigtail, Straight, Curved) at an affordable price in the global market. These stents are thoughtfully designed with small pigtails to ensure secure retention within the biliary system. Made from a soft radiopaque polyurethane substance, these stents provide excellent visibility under imaging techniques, aiding in accurate placement and monitoring. MEDITECH DEVICES PVT LTD’s Biliary Stent (Pigtail, Straight, Curved) is a reliable and cost-effective solution for patients requiring biliary drainage, offering optimal performance and peace of mind.
Pancreatic Pseudocysts Stent for EUS Intervention
 Introducing the Innovative Pancreatic Pseudocysts Stent for EUS Intervention. Produced by Mitra Industries Private Limited. Mitra Industries Pvt. Ltd., a renowned manufacturer and global supplier headquartered in India, proudly unveils its state-of-the-art solution for managing pancreatic pseudocysts through endoscopic ultrasound (EUS) interventions. This meticulously crafted stent is engineered to precision to cater to the specific needs of healthcare professionals worldwide.
Introducing the Innovative Pancreatic Pseudocysts Stent for EUS Intervention. Produced by Mitra Industries Private Limited. Mitra Industries Pvt. Ltd., a renowned manufacturer and global supplier headquartered in India, proudly unveils its state-of-the-art solution for managing pancreatic pseudocysts through endoscopic ultrasound (EUS) interventions. This meticulously crafted stent is engineered to precision to cater to the specific needs of healthcare professionals worldwide.
Mitra Industries Pvt. Ltd., acknowledged for its prowess in stent production, guarantees exceptional quality and dependable products. The specialized stent boasts a protective shield that prevents leaks and tissue overgrowth, thereby enhancing patient safety and minimizing potential complications. Its broad and precisely angled flares provide unparalleled resistance against migration, ensuring accurate placement and sustained efficacy over time.
Furthermore, the stent’s generous diameter facilitates the safe and effortless removal of pancreatic necrosis, streamlining drainage procedures for optimal outcomes.”
Conclusion
In this comprehensive guide, we have embarked on a captivating exploration of the world of stents and their remarkable impact on modern medicine. Through a step-by-step understanding of stent placement, removal, and insertion procedures, we have empowered patients and caregivers with valuable insights and knowledge. Moreover, we have recognized the significance of managing stent complications, addressing migration and thrombosis risks, and staying updated with the latest advancements in the field. We have also shed light on the long-term effects of stent placement and the importance of comparing different stent types for informed decision-making.